Periodontal preparation
Periodontal preparation is usually performed in the period following oral surgical procedures. However, when the patient’s calculus accumulation is excessive, it is advisable to perform a gross debridement before tooth extraction to avoid causing infection. Periodontal treatment must be completed before restorative treatment. The remaining teeth, especially those with RPD abutments, should be evaluated for periodontal support and treated.
Periodontal therapy aims to restore the health of the teeth’s supporting tissues and establish an environment that allows the periodontium to be preserved.
In order to meet this goal, the following particular requirements must be met:
- Removing and controlling etiologic factors that cause periodontal disease,
- Ensuring a healthy gingival groove by reducing or eliminating pocket depths,
- Achieving a non-traumatic, functional occlusal relationship and tooth stability,
- Establishment of a customized plaque control program and a clear maintenance plan.
Strengthening teeth with weak periodontal support (Splinting)
Some or all of the teeth present in the mouth may have poor periodontal support and require splinting to provide healthy support and stability for the RPD. Splinting can be fixed or removable.
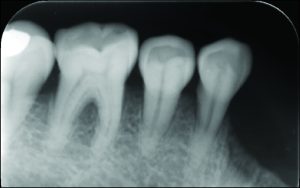
Crown restorations that are joined together provide fixed splinting. When force is applied, the goal is for the teeth to resist one another. Anteroposterior resistance is increased when the posterior support teeth are splinted. The posterior restoration needs to incorporate multiple anterior teeth in order to be effective in the mediolateral direction (Figure 10-12).

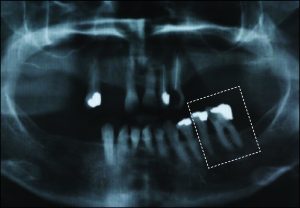
Fixed splinting in such a situation weakens the support of the healthy tooth instead of strengthening the weak abutment tooth. RPD further complicates the situation and accelerates tooth loss. The best treatment option in this case might be to extract the weak abutment tooth and use the adjacent abutment tooth as RPD primary abutment.
The use of direct retainers on isolated abutment teeth in distal extension PRD cases usually accelerates the destruction of the periodontium, leading to tooth loss. For this reason, it is recommended to place rests on isolated teeth and not to use direct retainers. Another option is restoration of the modification space with a fixed partial denture and splinting of the teeth (Figures 10-15).
Posterior teeth that have lost some of their periodontal support are strategically significant in tooth supported RPDs having long edentulous residual crests. When the posterior abutment teeth are not available to achieve retention, distal extension denture base rotation would occur in response to masticatory forces. However, by using just occlusal rests without clasps, the posterior tooth support minimizes the denture base embedding and gives the prosthesis a tooth-supported character. Both patient satisfaction and prosthetic function might be enhanced by this modification in treatment planning.